Workflow adopted by the National Cervical Cancer Screening Programme2 for women who are 30 years and above
Let's talk cervical cancer prevention

Regular screening and timely HPV vaccination are key to preventing cervical cancer1. Encouraging friends to take action can make a big difference.
Talking to friends and those you love about cervical cancer screening or HPV vaccination can feel a little awkward. Here are some conversation starters—what’s yours?
I really care about you. Have you had your regular check-up or cervical screening recently?
Did you know that both HPV vaccination and cervical screening can prevent cervical cancer? Your doctor can guide you on what’s right based on your age and history.
Have you talked to your doctor about HPV vaccination? It’s a great way to protect against cervical cancer—especially when done early.
- I just booked my cervical screening—it reminded me to check in with you too. Want help finding a clinic or making an appointment?
- Regular cancer screening is really important. Is there anything I can do to help you get screened, like find information, schedule an appointment, help with the kids or drive you to the clinic?
References
- https://www.who.int/news-room/fact-sheets/detail/cervical-cancer
Let's talk about cervical cancer screening
What is cervical cancer? Why should a woman care?
Cervical cancer is one of the most common cancers in women worldwide. It starts in the cervix, located at the lower part of the uterus. Persistent infection of certain high-risk types of the HPV virus are known to increase the risk of cervical disease. Cervical disease, if left unchecked can progress over time to cervical cancer. Cervical cancer is one of the most successfully treatable forms of cancer, as long as it is detected early and managed effectively.1

What's the link between HPV and cervical cancer?
Human papillomavirus (HPV) is a common virus that is primarily transferred by skin-to-skin sexual contact. In fact, HPV is so common that over 80% of sexually active adults will get HPV at some point in their lives.2
While over 150 types of HPV have been identified, only some are high-risk HPV types, known to cause health problems such as genital warts and cancers. Testing positive for HPV is not a negative reflection on you, your partner, or your lifestyle.
There is no treatment for the HPV virus. Most high-risk HPV infections have no symptoms, are harmless, and are cleared by the body’s immune system within two years.3 Since there are often no symptoms, a woman may never know that she or her partner has HPV. However, when the presence of HPV continues, certain types of high-risk HPV can progress to precancer or cancer. In women, HPV 16 and HPV 18 are the two highest risk types, known to cause close to 70% of cervical cancer cases.5

Over 80% of sexually active adults will get HPV at some point in their lives2

Most HPV infections are transient3

Around the world, cervical cancer is one of the most common cancers in women4

70% of cervical cancers are caused by the two highest risk types, HPV 16 & HPV 185
References
- https://www.who.int/health-topics/cervical-cancer#tab=tab_1
- Chesson, HW et al, Sex Transm Dis. 2014;41(11):660–4
- Lim TSC, Ismail-Pratt I, Goh LH. Cervical cancer screening and vaccination: understanding the latest guidelines. Singapore Med J. 2022 Mar;63(3):125-129.
- Human papillomavirus (HPV) and cervical cancer 24 January 2019. https://www.who.int/en/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer
- Li, N et al, Int J Cancer. 2011;128(4):927–35
Let's talk about booking your cervical screening appointment.
Getting screened for HPV and cervical cancer is one of the most important things you can do for your health. All women above a certain age, even those in monogamous relationships or with the same long-term partner, need to be tested for HPV. A positive test result doesn't indicate when you got the infection or from whom, and some research suggests that HPV can lay dormant for some time.1 Testing positive is not a reflection on you, your partner or your lifestyle. So, while testing HPV positive doesn't necessarily mean you have, or will develop cervical cancer, it does mean you could be at an increased risk. It's important to know which HPV type you have to fully understand your risk.
Even if you received the HPV vaccine, you should still be screened for cervical cancer.
Although the available HPV vaccines cover some high-risk HPV types (including HPV 16 and HPV 18, the two highest risk types), they do not cover all high-risk HPV types. Therefore, experts still recommend that you continue to get screened regularly for cervical cancer even after you’ve received the vaccine.6
PAP Test VS HPV DNA Test: Consult your healthcare provider
Pap Test |
HPV DNA Screening |
|
| Clinician-collected only4 | Specimen collection |
Clinician-collected4 or self-collected4 |
| Looks for abnormal changes in cervical cells7 using a microscope4 | Purpose |
Identifies the presence of high-risk HPV strains even before cervical cell changes occur12 |
| A sample is taken from the cervix and examined for abnormalities13 | Sample type |
A sample can be taken from either the cervix14 or vagina and checked for the presence of HPV11 |
| 25-29 years old4 | Age
|
30-69 years old4 |

Self-collection for cervical screening is easy and comfortable!
You can prevent cervical cancer before it starts .
One case of cervical cancer that could have been prevented is one case too many.
Cervical cancer affects more than 200 women annually in Singapore. Early detection and regular cervical screening makes cervical cancer highly preventable and curable6.
HPV DNA screening and Pap test are a part of cervical screening.
Pap test, also known as Pap Smear or Cytology, looks for cell changes on the cervix that may develop to cervical cancer7.
On the other hand, HPV DNA screening detects HPV infection, as persistent HPV infections with high-risk HPV strains can increase your risk of cervical cancer8. It will be able to detect cervical cancer at its pre-cancer stage9. This is why cervical cancer is known to be a highly preventable cancer10.
Women who have had sex in the past or present, are advised to start cervical screening from the age of 25 and those above the age of 30 are encouraged to go for a HPV DNA screening every 5 years as recommended by the National Cervical Screening Programme in Singapore4. For HPV DNA screening, you may opt for your healthcare provider to collect a sample or you may choose to collect your own sample.
Are you eligible to collect your own sample for cervical screening?
Self-collection for cervical screening is an option to be considered for women who are:

30 years old and above4

Sexually active or have been sexually active11

Not pregnant11
The above is not an exhaustive list. Speak to your healthcare provider to understand better if collecting your own sample for a HPV DNA screening is the right option for you. Your healthcare provider will provide personalised recommendations and further information pertaining to cervical screenings.
How to collect your own sample for HPV DNA screening
If you have decided to collect your own vaginal sample for HPV DNA screening, do inform your healthcare provider about your choice.
Your healthcare provider will explain how to collect your own sample and hand you a self-collection kit.

Wash your hands with soap

Your doctor or nurse will hand a swab and a bottle with a clear solution.

Turn cap to remove swab.

Hold the swab at the red marking, do not touch the tip of the swab.

Stand or sit in a comfortable position.

Insert swab until your fingers at vagina opening.

Rotate swab.

Carefully uncap the bottle with a clear solution.

Swirl swab while ensuring that it remains fully immersed.

Drain fluid from the swab.

Return swab and bottle to your healthcare provider.
Get comfortable when collecting your own sample
You may choose to stand or be seated when collecting your own vaginal sample as you should feel comfortable during the self-collection process.
Here are some positions you can get into to help you with collecting your own vaginal sample.
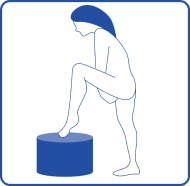
Standing
Stand with one leg raised to rest your one leg on a stool15.

Seated
Sit on the toilet bowl with your legs slightly spread open15.
How do I know if I’m collecting my sample correctly?
Follow the step by step guide provided by your healthcare provider.

It’s been a couple of years since Eva last did a cervical screening test. Upon returning to the doctor this time, she was advised to keep up with regular screenings. Since Eva has 2 kids and a busy schedule, her doctor recommended that she get a self-collection kit so she did not need to wait for a doctor’s examination.
With a few explanations from the helpful nurse, Eva was able to easily collect her sample at the GP. This self-collection method offers Eva a private and accessible way to prioritise her own health and well-being despite her packed schedule.
By performing a self-collected sample for cervical screening, Eva can take proactive measures and seek timely medical attention if necessary, ensuring early detection and better chances of successful treatment.
Take action now, get screened today.
Schedule your cervical screening appointment today
Cervical screening is conveniently available at:
- Major health screening centres
- Most primary care and General Practitioner (GP) clinics
- Obstetrics and Gynaecology (O&G) clinics at major private and public hospitals
The Singapore Cancer Society provides cervical screening at no cost for eligible candidates. Subsidised screening is also available at Polyclinics and Community Health Assist Scheme (CHAS) clinics for women who are eligible.
Speak to your healthcare provider to find out if self-collection for HPV DNA screening is an option for you, or visit your nearby clinic to learn more.

Frequently Asked Questions
Can viral infections such as HPV really lead to cancer?
Persistent HPV infection with high-risk strains is the cause of 99.7% of cervical cancer cases¹⁷. HPV is a common infection with at least 4 out of 5 women would have had a HPV infection by the age of 50¹⁸. The virus is transmitted through skin-to-skin contact such as through sexual intercourse¹⁹.
Most HPV infections resolve by themselves within two years but some of them can last longer and cause cancer including cervical cancer²⁰. It takes about 15 to 20 years for cervical cancer to develop among women with a normal immune system⁸.
HPV DNA screening can help with early detection and prevention of cervical cancer by detecting the presence of HPV, including high-risk HPV strains¹⁴.
Will a healthcare provider explain to me about my self-collected cervical screening test results?
It is important to speak with your healthcare provider about your self-collected cervical screening result. This conversation is essential to help you understand what the results mean and whether any follow-up is needed.
If your HPV DNA screening results are negative, you will be advised to repeat the HPV DNA screening in 5 years⁴.
On the other hand, if your HPV DNA screening results are positive or abnormal, this indicates that the screening has identified the presence of HPV²¹ but it is important to take note that a HPV DNA screening does not directly indicate if you have cancer¹⁴. Instead, it identifies the presence of HPV, including high-risk HPV strains that increase your risk of developing cervical cancer¹⁴. You may be required to return for a Pap test²¹, which looks for abnormal changes in the cervical cells¹⁴.
(The information provided is for educational purposes only and does not substitute for professional medical advice)
Can a healthcare provider collect my sample for the HPV DNA screening instead of me?
Sure, the choice is yours. Speak to your healthcare provider if you prefer to have your healthcare provider collect your sample for your HPV DNA screening.
How does a woman know if she has cervical cancer?
During the early stages of cervical cancer, there are no symptoms²². Symptoms of cervical cancer such as vaginal bleeding between periods and pelvic pain during sex usually present itself after the cancer has progressed²³.
One way to detect cervical cancer at its early stage is through a cervical screening. Through this screening your healthcare provider will be able to identify early changes in the cells as well as the presence of HPV strains. As a matter of fact, cervical screening can detect cervical cancer at its pre-cancer stage, hence making it possible for you to prevent it⁹.
Is the swab for collecting my sample a ‘one-size-fits-all’?
The provided swab is a vaginal swab, designed for easy and comfortable self-collection. Simply follow the step-by-step instructions provided by your healthcare provider to get correct results and avoid having to repeat the test.
What happens if my self-collected HPV test results are positive?
You will be asked to return to your healthcare provider so that a sample can be collected by your healthcare provider for further screening²⁰. If HPV strains 16 and 18 were detected (these strains are responsible for 70 percent of cervical cancers)²⁴ in your HPV DNA screening results, your healthcare provider will follow-up with another type of test for cervical screening, known as colposcopy. If other HPV strains were detected, a Pap test will be conducted and the next steps will be advised accordingly depending on the results²¹.
If I am in a wheelchair, will it be possible for me to consider collecting my own vaginal sample for HPV DNA screening?
There are suggestions that self-collection for HPV DNA screening might be an option as there is no need for a speculum examination. If you are in a wheelchair or with disabilities, it would be best for you to discuss with your healthcare provider about the option to collect your own vaginal sample for cervical screening ²⁵.
How can I prevent cervical cancer?
Cervical cancer is one of the most preventable cancers¹⁰. Some steps you can take to reduce your risk of developing cervical cancer includes:
- Getting vaccinated against HPV²⁶.
- Attending your routine cervical screening²⁶.
- Follow through with the necessary screening and steps as guided by your healthcare provider if your cervical screening results are abnormal²⁶.
References
- Rositch AF, Burke AE, Viscidi RP, Silver MI, Chang K, Gravitt PE. Contributions of Recent and Past Sexual Partnerships on Incident Human Papillomavirus Detection: Acquisition and Reactivation in Older Women. Cancer Res. 2012;72(23):6183–90.
- Walboomers JMM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathology. 1999;189(1):12–9.
- https://www.cancer.gov/publications/dictionaries/cancer-terms/def/pap-test (accessed 13 January 2021).
- https://sccps.org/wp-content/uploads/2025/03/Cervical-Cancer-Screening-Clinical-Management-Guidelines-2025.pdf
- Centers of Disease Control and Prevention. “What are the risk factors for cervical cancer?”. https://www.cdc.gov/cancer/cervical/basic_info/risk_factors.htm#:~:text=Almost%20all%20cervical%20cancers%20are%20caused%20by%20human %20papillomavirus%20(HPV,cause%20genital%20or%20skin%20warts. (accessed on September 19, 2023)
- Singhealth. “Cervix cancer/cervical cancer-What it is”. https://www.singhealth.com.sg/patient-care/conditions-treatments/cervix-cervical-cancer#:~:text=Cervical%20cancer%20is%20the%2010th,in%20causing%20most%20cervical%20cancer (accessed 19 November 2023).
- Centers of Disease Control and Prevention. “What should I know about cervical cancer screening?”. https://www.cdc.gov/cancer/cervical/basic_info/screening.htm#:~:text=The%20HPV%20test%20looks%20for,they%20are%20not%20treated %20appropriately. (accessed on 30 October 2023).
- World Health Organization. “Cervical Cancer”. https://www.who.int/news-room/fact-sheets/detail/cervical-cancer#:~:text= It%20takes%2015%20to%2020,those%20with%20untreated%20HIV%20infection. (accessed 26 October 2023).
- Cancer.net. “Cervical cancer: Screening and prevention”. https://www.cancer.net/cancer-types/cervical-cancer/screening-and-prevention (accessed on September 19, 2023).
- Centers for Disease Control and Prevention. “Cervical Cancer Highly Preventable” https://www.cdc.gov/vitalsigns/cervical-cancer/ndex.html#:~:text=Up%20to%2093%25%20of%20cervical,that%20cause%20most%20cervical%20cancers (accessed on September 19, 2023).
- Australian Government Department of Health and Aged Care. “Self-collection for the cervical screening test”. https://www.health.gov.au/self-collection-for-the-cervical-screening-test (accessed on 18 October 2023).
- American Cancer Society. “HPV and HPV Testing”. https://www.cancer.org/cancer/risk-prevention/hpv/hpv-and-hpv-testing.html#:~:text=The%20HPV%20test%20looks%20for,risk%20of%20developing%20cervical%20cancer. (accessed 8 November 2023)
- WebMD. Pap Smear”. https://www.webmd.com/women/pap-smear (accessed 8 November 2023)
- Mayo Clinic. “HPV Test”. https://www.mayoclinic.org/tests-procedures/hpv-test/about/pac-20394355 (accessed on 17 October 2023)
- Canadian Family Physician. “Clinician acceptability of self-collected human papillomavirus swabs as a primary cervical cancer screening method”. https://www.cfp.ca/content/68/2/e31 (accessed on 19 November 2023).
- National Library of Medicine. “HPV-Based Self-Sampling in Cervical Cancer Screening: An Updated Review of the Current Evidence in the Literature”. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10046242/ (accessed on 19 November 2023).
- National Library of Medicine. “Human papillomavirus and cervical cancer”. https://pubmed.ncbi.nlm.nih.gov/31500479/#:~:text=Cervical%20cancer%20is%20by%20far,human%20papillomavirus%20(HPV)%20infection. (accessed 26 October 2023).
- Centers of Disease Control and Prevention. “Basic information about cancer and HPV”. https://www.cdc.gov/cancer/hpv/basic_info/index.htm#:~:text=By%20age%2050%2C%20at%20least,and%20often%20has%20no%20symptoms. (accessed on 26 October 2023).
- Centers of Disease Control and Prevention. “HPV infections are common”. https://www.cdc.gov/hpv/parents/about-hpv.html#:~:text=Nearly%20everyone%20will%20get%20HPV,teens%2C%20become%20infected%20each%20year. (accessed 17 October 2023).
- Centers of Disease Control and Prevention. “HPV infections are common”. https://www.cdc.gov/hpv/parents/about-hpv.html#:~:text=Nearly%20everyone%20will%20get%20HPV,teens%2C%20become%20infected%20each%20year. (accessed 17 October 2023).
- National Cervical Screening Program. “Understanding the National Cervical Screening Program Management Pathway: A Guide for Healthcare Providers”. https://www.health.gov.au/sites/default/files/documents/2022/07/national-cervical-screening-program-understanding-the-national-cervical-screening-program-management-pathway.pdf (accessed on September 19, 2023).
- Health Hub. “Cervical cancer”. https://www.healthhub.sg/a-z/diseases-and-conditions/topic_cervical_cancer (accessed 8 November 2023)
- National Cancer Institute. “Cervical Cancer Symptoms”. https://www.cancer.gov/types/cervical/symptoms (accessed on September 19, 2023).
- National Library of Medicine. “Prevalence of Human Papillomavirus subtypes 16 and 18 among Yemeni Patients with Cervical Cancer”. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6373819/#:~:text=HPV%20types%20(16%20and%2018,ca
rcinogenic%20than%20other%20HPV%20types (accessed on September 19, 2023). - National Library of Medicine. “Cervical Cancer Screening for Women With Disabilities: Time for a New Approach?” https://pubmed.ncbi.nlm.nih.gov/30161053/ (accessed 19 November 2023).
- Centers for Disease Control and Prevention. “What can I do to reduce my risk of cervical cancer?” https://www.cdc.gov/cancer/cervical/basic_info/prevention.htm. (accessed on September 19, 2023).
- Arbyn et al BMJ 2018; 363 doi: https://doi.org/10.1136/bmj.k4823 (accessed 19 November 2023).
Let's talk about your cervical screening results and the next steps
Understanding your Pap smear results2
If your Pap smear result is normal, it means no abnormal cells were found, and you should continue regular screening every 3 years. If the result is unsatisfactory, your doctor might ask you to repeat the test. If the result is abnormal, it does not mean you have cancer, but some changes were found in your cervical cells. Your doctor may recommend a follow-up test, such as another Pap smear, an HPV test, or a colposcopy. Always speak to your doctor to understand what your result means and what you should do next.
Understanding your primary HPV screening test results
HPV screening can help your healthcare provider identify if you are at risk2 for cervical cancer. If you receive a positive test result, it’s normal to feel anxious or worried. However, it’s important to remember that a positive HPV test result does not automatically mean that you already have, or will develop, cervical cancer. Talk to your healthcare provider, who will discuss next steps with you.
Dependent on your results2 you’ll be asked to:
- Have some more tests
- Come back for cervical screening in 1 year
- Come back for cervical screening in 3 years
- Come back for cervical screening in 5 years
Breaking down the stigma surrounding HPV and cervical cancer
A positive HPV result does not necessarily mean you or your partner have been unfaithful, as the virus can stay dormant (latent) for years before an infection is detected. Having HPV is not a reflection on you, your partner or your lifestyle and it isn't something to be ashamed or afraid of. The majority of men and women with a healthy, active sex life will be exposed at some point, and may never know it. In most cases, the infection has no symptoms, and usually resolves on its own without causing a problem. However, <10%3 of women will test positive for HPV, and of those, some may develop cervical disease if an HPV infection is left undetected and untreated.
We have the power to protect cervical health
Every year >600,000 4 women are diagnosed with cervical cancer globally - this disease is highly preventable. With a combination of vaccination, advances in screening and appropriate treatment, cervical disease can be found and stopped. The goal is to identify women at risk, before invasive cancer ever develops. We have the power, by helping to spread the word about the role of Human Papillomavirus (HPV) in the cause of cervical cancer, to protect women from this preventable disease.
References
- https://www.canceraustralia.gov.au/affected-cancer/cancer-types/cervical-cancer/preventing-cervical-cancer
- Cervical Screen Singapore. “Management Guidelines for Cervical Screening & Preinvasive Disease of the Cervix”. https://sccps.org/wp-content/uploads/2025/03/Cervical-Cancer-Screening-Clinical-Management-Guidelines-2025.pdf
- Self-sampling HPV DNA test for cervical cancer screening in Singapore: A prospective study https://doi.org/10.47102/annals-acadmedsg.2022133
- https://www.thelancet.com/journals/langlo/article/PIIS2214-109X%2822%2900501-0/fulltext
- Ebisch, R., van der Horst, J., Hermsen, M. et al. Evaluation of p16/Ki-67 dual-stained cytology as triage test for high-risk human papillomavirus-positive women. https://doi.org/10.1038/modpathol.2017.16
Let’s talk about empowering women

What is National Women’s Checkup Week?
National Women’s Checkup Week (NWCW) is an awareness initiative with a dedicated call-to-action to remind women of all ages to prioritise their cervical health by scheduling regular check-up appointments with their healthcare providers.
Key facts about cervical cancer:
- Each year, more than two million women are diagnosed with cervical or breast cancer.1
- Cervical cancer is one of the most preventable cancers, yet it still affects thousands of women every year2.
By getting screened regularly, the risk of developing cervical cancer, and other forms of cancer, can be significantly reduced.

Cervical screening status in Singapore

The top reasons for skipping cervical screening are that 23% of women believe nothing is wrong, and 21% report a lack of information on where to get screened5.
The top reasons for skipping cervical screening are that 23% of women believe nothing is wrong, and 21% report a lack of information on where to get screened5.
Reason For Not Having Screening

At a Glance
- Since 2023, Roche has championed the #EveryWoman initiative to ensure all women have access to early and accurate health screenings.
- The #THEMOSTIMPORTANTDATE movement aims to empower women to take control of their health by collaborating with community groups, businesses, and healthcare providers.
- National Women's Checkup Week will run in May, with activities planned during the month.
Campaign Materials
We invite all national, local, and community organisations passionate about empowering women to better look after their physical health to join us in the movement
Additional suggestions
- Use #MakeTheMostImportantDate and #ShowUpForHerHealth hashtags on your social channels during the National Women Checkup Week to join the conversation and share information, pictures and videos.
- Share messages with suggested graphics or your own images, GIFs, and videos.
- Customise messages that may help your messages reach your target audience.
- Email [email protected] for the National Women’s Checkup Week toolkit which includes social media assets, posters, digital banners and videos.




National Women’s Checkup Week is a meaningful opportunity to highlight the importance of regular health screenings in supporting women’s long-term health. By taking part in this national effort, we can help encourage more women in Singapore to prioritise their health and well-being through timely checkups.
Our Partners
Activ.Co
Care Family Clinic
Finest Health Medical Centre
Healthmark Family Clinic
Pinnacle Family Clinic
Parkway Laboratories
Pathlab Singapore
Singapore Cancer Society
Straits Clinic Anchorpoint
Tampines Family aMedicine Clinic
References
- Ginsburg O, Bray F, Coleman MP, Vanderpuye V, Eniu A, Kotha SR, Sarker M, Huong TT, Allemani C, Dvaladze A, Gralow J, Yeates K, Taylor C, Oomman N, Krishnan S, Sullivan R, Kombe D, Blas MM, Parham G, Kassami N, Conteh L. The global burden of women's cancers: a grand challenge in global health. Lancet. 2017 Feb 25;389(10071):847-860. doi: 10.1016/S0140-6736(16)31392-7. Epub 2016 Nov 1. PMID: 27814965; PMCID: PMC6191029.
- Ginsburg O, Bray F, Coleman MP, Vanderpuye V, Eniu A, Kotha SR, Sarker M, Huong TT, Allemani C, Dvaladze A, Gralow J, Yeates K, Taylor C, Oomman N, Krishnan S, Sullivan R, Kombe D, Blas MM, Parham G, Kassami N, Conteh L. The global burden of women's cancers: a grand challenge in global health. Lancet. 2017 Feb 25;389(10071):847-860. doi:
- 10.1016/S0140-6736(16)31392-7. Epub 2016 Nov 1. PMID: 27814965; PMCID: PMC6191029.
- Bruni L, Albero G, Serrano B, et al. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in Singapore. Summary Report, 10 March 2023. https://hpvcentre.net/statistics/reports/SGP.pdf. Accessed 11 May 2024.
- Roche Diagnostics Asia Pacific Women’s Health Survey 2024 (Data on file)
- World Economic Forum. Women’s cancer is getting worse in the Asia Pacific – here’s what we can do. Available via: https://www.weforum.org/stories/2023/10/womens-cancer-is-getting-worse-in-asia-pacific-heres-what-to-do/
- International Agency for Research on Cancer. World Health Organisation. GLOBOCAN (Cervix Uteri). Available via: https://gco.iarc.who.int/media/globocan/factsheets/cancers/23-cervix-uteri-fact-sheet.pdf
- SG Survey link: https://docs.google.com/presentation/d/1TfGNju7dfYDJFxI-g2wB0ahblX6qdIMjNNnp_Tvshj4/edit#slide=id.g2b010a354a3_1_0
Appendix
Terms and conditions for use of National Women's Check-up Week campaign (the "Campaign") logo and materials (collectively, "Promotional Assets")
- Promotional Assets may be used by Roche's designated Campaign partners (i) solely to promote, and/or provide education and information on the Campaign, and (ii) for the duration of the Campaign only. Such use must be consistent with the Campaign's goals, these terms and conditions, and any identity guide provided by Roche Diagnostics Asia Pacific ("Roche").
- Designated Campaign partners may add their organisational logos to the Promotional Assets if they retain the words "National Women’s Checkup Week" and the Campaign logo. They may not, however, add other logos (e.g. product logos) to the Promotional Assets, or change the Promotional Assets in any way, without the permission of Roche.
- All rights in the Promotional Assets are owned by Roche. Other than as stated in these terms and conditions, the Promotional Assets may not be used without Roche's express written consent. All designated Campaign partners must include the following copyright notice clearly and prominently when sharing the Promotional Assets in public "© (2023) Roche Diagnostics Asia Pacific". The designated Campaign partner shall not, and shall ensure that its employees and contractors do not, register any trademark containing the Campaign name, logo, or visual element developed in any language or media.
- Roche's permission to use the Promotional Assets according to these terms and conditions does not include any permission to use Roche's name, logo, or any other intellectual property owned and/or controlled by Roche. Roche's permission also does not mean that there is any affiliation or association between Roche and the designated Campaign partner, or that Roche has endorsed the designated Campaign partner's views, opinions, or activities. Roche's designated Campaign partner must not use the Promotional Assets, or behave in any manner that disparages Roche, and/or harms Roche's goodwill and reputation.
- Roche may revoke the right to use the Promotional Assets at any time without any further explanation, including in the event that these terms and conditions are not complied with.
- All Promotional Assets are shared on an "as is" basis only. Roche cannot be liable for the use of such Promotional Assets by the designated Campaign partner or any other party.
Let’s talk about finding additional resources about cervical screening
Cervical cancer prevention begins with education, HPV awareness and access to women’s wellness resources that can help you be proactive about your health. Swipe or scroll below to see the valuable resources offered by many different organizations in Singapore and around the world.
Information on booking for your free HPV test for cervical cancer screening

