For localized information and support, would you like to switch to your country-specific website for {0}?
COVID-19 is here to stay
The efforts to manage the pandemic have led to an unprecedented technological development culminating in the largest vaccination campaign in history.1 The World Health Organization (WHO) has granted emergency use listing for 11 vaccines2 and over 13 billion doses have been administered globally.3 In its first year, the vaccination campaign was estimated to have saved around 20 million lives.4 Furthermore, hundreds of diagnostic tests, including antibody, antigen and polymerase chain reaction (PCR) tests, were developed in record time.5
While it is generally believed that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) will become endemic and vaccines will provide protection from severe disease and death, a lot of uncertainty remains. First, predicting the evolutionary course of SARS-CoV-2 variants is exceedingly difficult due to the overlayed complexity of pre-existing immunity.6 Second, our understanding of the innate and adaptive immunologic mechanisms associated with coronavirus disease 2019 (COVID-19) is still incomplete.7,8 COVID-19 is here to stay, and there will still be an ongoing need for new treatments and diagnostics.
As of February 17, 2023, COVID-19 has claimed over 6.8 million lives
There have been over 760 million confirmed cases worldwide3

Patient-centricity – a hallmark of COVID-19 management in the future
Understanding of the immunologic responses in these populations at risk for severe COVID-19 is central to making better informed decisions on COVID-19 management, in the context of regular clinical care and could be ascertained by development of new testing strategies.
As the COVID-19 pandemic transitions to endemicity, understanding of the immunologic mechanisms underlying SARS-CoV-2 immunity in patients at high risk of severe COVID-19 becomes increasingly important (data as of February 17, 2023).1,3‑5,9‑11
It is well known that the risk of severe COVID-19 increases with age and pre-existing comorbidities
About one in five individuals could be at an increased risk of severe COVID-19 due to an underlying health condition, with disorders of the immune system (genetic immune defects; immunosuppressive therapy; medical conditions like cancer, HIV/AIDS, or chronic inflammatory conditions) being a key contributing risk factor9-12

A holistic understanding of immunity against COVID-19 is key
The immune system provides protection from countless pathogens that are constantly evolving. B and T lymphocytes are the two major pillars of the adaptive immune response [Video].
The role of the adaptive immune system
Although vaccination reduces SARS-CoV-2 infection-related morbidity and mortality, emerging variants may have decreased susceptibility to antibody-mediated neutralization.13,14 As SARS-CoV-2 is likely to continue evolving, we must use every tool at our disposal to enable normal social functioning while protecting individuals from severe disease and death. To accomplish this goal, a comprehensive understanding of the adaptive immune response to SARS-CoV-2 is needed.13 This understanding could be facilitated by development of new COVID-19 diagnostic tools for routine use (Figure 1).
Figure 1. COVID-19 unmet diagnostic needs: an assay that determines protection from infection following vaccination or re-infection after past infection13,15-21

Binding antibody assays generally cannot differentiate between
neutralizing and other antibodies, yet may show a good correlation depending on assay design15

Decrease in IgG levels and nAbs has been observed in recovered
individuals at different extent and speed, possibly depending on the assay employed and intrinsic patient differences16–18

There is limited knowledge on how SARS-CoV-2-specific humoral or
cellular immunity mediates durable protection19
nAb antibody titers are highly predictive of immune protection from symptomatic SARS-CoV-2 infection20

Some patients fail to develop high titers of nAbs after COVID-19 infection21

T-cell reactivity is therefore very important for individuals who are not able to mount a sufficiently strong antibody response13
A better understanding of cellular immunity is urgently needed to better predict disease outcome and determine whether patients develop long-lasting immunity
Abbreviations: COVID-19, coronavirus disease 2019; IgG, immunoglobulin G; nAbs, neutralizing antibodies; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2
During COVID-19 vaccine development the role of neutralising antibodies (nAbs) has been a major focus and less emphasis has been applied on understanding the role of T cells, memory B cells, and non-nAbs that may confer protection.13 As both humoral and cellular immunity collaborate for pathogen control, the development of a holistic understanding of the host response to pathogens like SARS-CoV-2 requires assessment of both antibodies and T cells.13
T-cell responses are less likely to be affected by virus variants. T-cell epitopes are derived from many viral antigens, including those that are under less selection pressure, while nAbs are predominantly targeting the spike protein. The spike protein shows a high number of mutations in emerging variants. T-cell responses are not only directed against spike but also the membrane, nucleocapsid, as well as non-structural proteins. In fact, >90% of CD4 + and CD8 + epitopes are 100% conserved across variants (including Omicron), and T cells of exposed donors or vaccinees effectively recognize SARS-CoV-2 variants (including Omicron).22-25
The Elecsys® IGRA SARS‑CoV‑2 assay for measurement of the T cell response complements Roche’s broad portfolio of COVID‑19 diagnostics
Elecsys® IGRA SARS-CoV-2 is an immunoassay for the qualitative detection of the T cell-mediated immune response to SARS-CoV-2. The assay is based on the ability of antigen-specific T cells to produce the pro-inflammatory cytokine IFN‑γ after encountering the antigen, which is a well-established marker of T-cell activation.13 IFN‑γ release assays (IGRA) employing similar principles have proven useful in tuberculosis where the Mycobacterium tuberculosis–specific IGRA test has replaced the previously used tuberculin skin test.13 The Elecsys® IGRA SARS-CoV-2 assay is intended as an aid in identifying individuals with an adaptive T cell response to SARS‑CoV‑2, indicative of past exposure to the virus or COVID-19 vaccination. It provides valuable information on the T cell responses of the patient, enabling the healthcare provider to make better informed decisions for patient care.
The assay uses a two-phased method to determine T cell immune response to SARS‑CoV‑2.


In vitro T cell stimulation using SARS-CoV-2-specific antigens in the cobas® IGRA SARS-CoV-2 Tubes: a fresh whole blood sample containing living T cells is incubated for 16–24 hours in the cobas® IGRA SARS-CoV-2 Tubes. Per patient sample, three different tube types are used: a Positive Control (PC) tube to determine the maximum T cell stimulation potential as a validation of sample quality; a Negative Control (NC) tube to determine the baseline IFN-γ level; and the specially coated Antigen tube to determine the IFN-γ released upon stimulation with SARS-CoV-2 peptides. The coating consists of 189 different peptides (the antigens) representing the SARS-CoV-2 membrane, nucleocapsid, spike, and non-structural proteins, providing a broad coverage of the SARS-CoV-2 genome. This peptide mix is designed to provide a substantial coverage (98%) of commonly occurring HLA subtypes to ensure that the response of both CD4+ and CD8+ T cells is captured. During the incubation, the stimulated SARS-CoV-2-specific T cells release IFN-γ, which is measured in the second phase.

IFN-y read-out using an automated electrochemiluminescence immunoassay (ECLIA): IFN-y released as a result of the T cell stimulation step is measured with the Elecsys® IGRA SARS-CoV-2 assay in plasma generated from the incubated blood samples. The numerical results from the NC tube, PC tube, and Antigen tube are evaluated in combination to derive the final qualitative result (T cell response detected or not detected).
The Elecsys® IGRA SARS-CoV-2 assay simplifies the determination of the cellular immune response to SARS-CoV-2 by automating a crucial part of the testing workflow.
It provides the physician with valuable information on the T-cell responses of their patients and can help inform clinical decisions in the next phase of the COVID-19 era. A better understanding of the holistic adaptive immune response in SARS-CoV-2-infected or -vaccinated individuals, and particularly the role played by T cells, will help future-proof our strategies against COVID-19. However, definitive verification for the protective role of T cells requires further research.13
Roche’s comprehensive response to the COVID-19 pandemic
There is now an increased global awareness of the value of diagnostic tests as public health tools.26
Roche is committed to finding innovative solutions to support the effective and accurate diagnosis of COVID-19, and offers a wide range of SARS-CoV-2 tests including the assessment of both antibody and T-cell responses.
Solutions cover both laboratory use and point-of-care (POC) tests that detect SARS-CoV-2 in currently infected patients or the patient’s immune response.

Figure 2. Roche’s extensive portfolio covers COVID-19 diagnostics across the disease continuum

Abbreviations: COVID-19, coronavirus disease 2019; POC, point-of-care; RAT, rapid antigen test; RT-PCR, reverse transcription-polymerase chain reaction; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; * Available in the US only, under an EUA
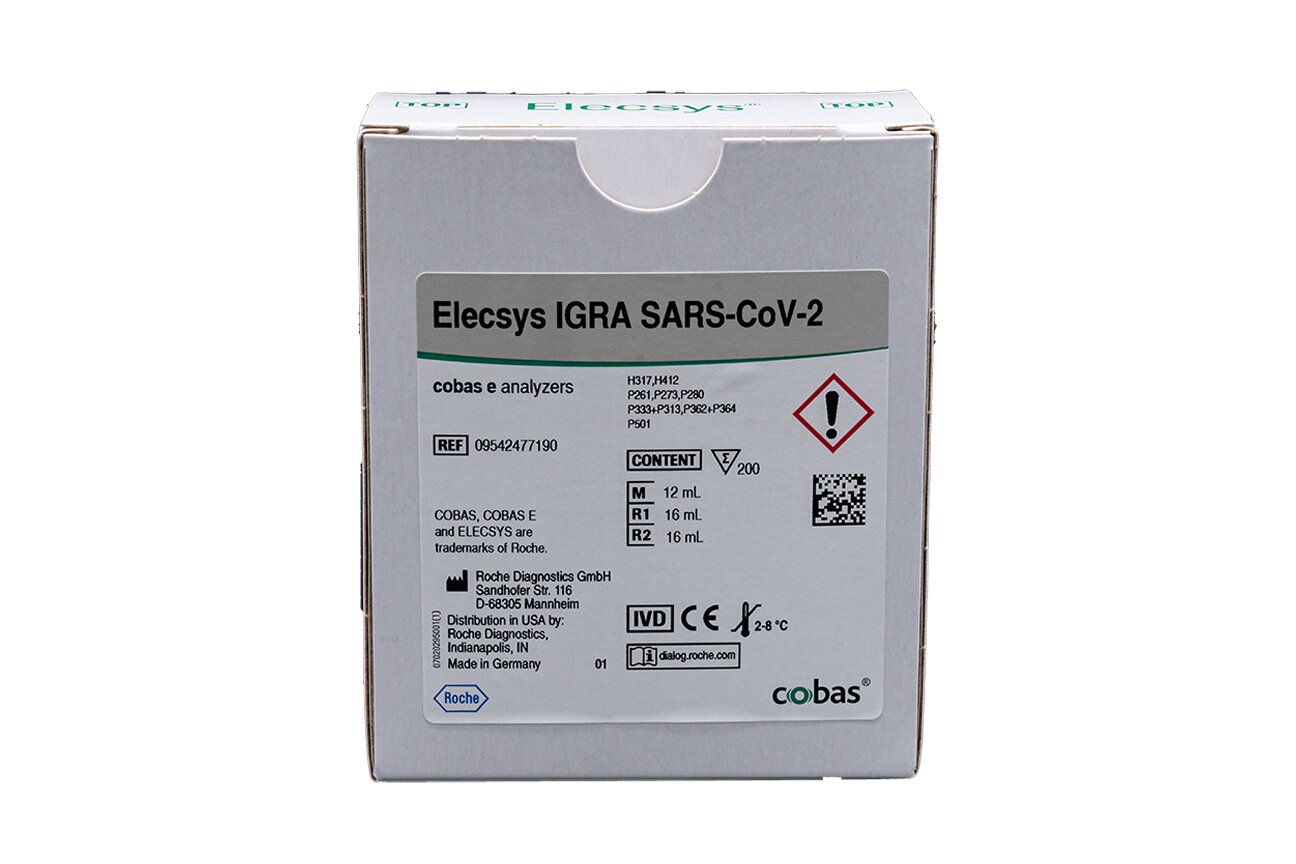
Elecsys® IGRA SARS-CoV-2
Elecsys® IGRA SARS-CoV-2
Learn more about how the Elecsys® IGRA SARS-CoV-2 assay can help to improve the understanding of the cellular immune response against SARS-CoV-2
References
- Tatar M, Wilson FA. The largest vaccination campaign in history: A golden opportunity for bundling public health interventions. J Glob Health. 2021;11:03076.
- World Health Organization. COVID-19 vaccine tracker [Internet; cited 2023 January 13]. Available from: https://covid19.trackvaccines.org/agency/who/.
- World Health Organization. WHO coronavirus (COVID-19) dashboard [Internet; cited 2023 February 17]. Available from: https://covid19.who.int/.
- Imperial College London. Vaccinations may have prevented almost 20 million COVID-19 deaths worldwide. [Internet; cited 2023 January 13]. Available from: https://www.imperial.ac.uk/news/237591/vaccinations-have-prevented-almost-20-million/.
- FIND Diagnostics for all. COVID-19 test directory. [Internet; cited 2023 January 13] Available from: https://www.finddx.org/covid-19/test-directory/.
- COVID is here to stay: countries must decide how to adapt. Nature. 2022;601(7892):165.
- Paludan SR, Mogensen TH. Innate immunological pathways in COVID-19 pathogenesis. Sci Immunol. 2022;7:eabm5505.
- Mohamed K, et al. COVID-19 vaccinations: The unknowns, challenges, and hopes. J Med Virol. 2022;94:1336-49.
- Clark A, et al. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Health. 2020;8:e1003-17.
- Shields AM, et al. COVID-19 in patients with primary and secondary immunodeficiency: the United Kingdom experience. J Allergy Clin Immunol. 2021;147:870-5.
- Figueroa-Parra G, et al. Risk of severe COVID-19 outcomes associated with rheumatoid arthritis and phenotypic subgroups: a retrospective, comparative, multicentre cohort study. Lancet Rheumatol. 2022;4:e765-74.
- MacKenna B, et al. Risk of severe COVID-19 outcomes associated with immune-mediated inflammatory diseases and immune-modifying therapies: a nationwide cohort study in the OpenSAFELY platform. Lancet Rheumatol. 2022;4:e490–506.
- Vardhana S, et al. Understanding T cell responses to COVID-19 is essential for informing public health strategies. Sci Immunol. 2022;7:eabo1303.
- Cele S, et al. Escape of SARS-CoV-2 501Y.V2 from neutralization by convalescent plasma. Nature. 2021;593:142-6.
- Montesinos I, et al. Neutralizing antibody responses following natural SARS-CoV-2 infection: Dynamics and correlation with commercial serologic tests. J Clin Virol. 2021;144:104988.
- Theel ES, et al. SARS-CoV-2 serologic assays dependent on dual-antigen binding demonstrate diverging kinetics relative to other antibody detection methods. J Clin Microbiol. 2021;59:e0123121.
- Long QX, et al. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat Med. 2020;26(8):1200-24.
- Wang X, et al. Neutralizing antibody Responses to severe acute respiratory syndrome coronavirus 2 in coronavirus disease 2019 inpatients and convalescent patients. Clin Infect Dis. 2020;71:2688-94.
- Baldanti F, et al. Choice of SARS-CoV-2 diagnostic test: challenges and key considerations for the future. Crit Rev Clin Lab Sci. 2022;2022:1-15.
- Khoury DS, et al. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat Med. 2021;27(7):1205-11.
- Boonyaratanakornkit J, et al. Clinical, laboratory, and temporal predictors of neutralizing antibodies against SARS-CoV-2 among COVID-19 convalescent plasma donor candidates. J Clin Invest. 2021;131:e144930.
- Grifoni A, et al. Targets of T cell responses to SARS-CoV-2 coronavirus in humans with COVID-19 disease and unexposed individuals. Cell. 2020;181:1489-501.
- Choi SJ, et al. T cell epitopes in SARS-CoV-2 proteins are substantially conserved in the Omicron variant. Cell Mol Immunol. 2022;19:447-8.
- Tea F, et al. SARS-CoV-2 neutralizing antibodies: longevity, breadth, and evasion by emerging viral variants. PLoS Med. 2021;18:e1003656.
- Tarke A, et al. Impact of SARS-CoV-2 variants on the total CD4+ and CD8+ T cell reactivity in infected or vaccinated individuals. Cell Rep Med. 2021;2:100355.
- Mercer TR, Salit M. Testing at scale during the COVID-19 pandemic. Nat Revs Gen. 2021;22:415-26.
- Roche. COVID-19 tests overview [Internet; cited 2023 January 13]. Available from: https://diagnostics.roche.com/global/en/c/covid-19-pandemic.html.
- Bonifacius A, et al. COVID-19 immune signatures reveal stable antiviral T cell function despite declining humoral responses. Immunity. 2021;54:340-6.
Video 1 references:
- Miller LE, Stevens CD. Clinical immunology and serology: a laboratory perspective. 5th edition. FA Davis Company; 2021.
- Abbas A, et al. Cellular and molecular immunology. 10th edition. Elsevier; 2021.
- Dash B, et al. Fundamentals of the immune system. In: Clinical immunodiagnostics: laboratory principles and practices. Jones & Bartlett Learning; 2020.
- Marshall JS et al. An introduction to immunology and immunopathology. Allergy Asthma Clin Immunol. 2018;14(Suppl 2):49.