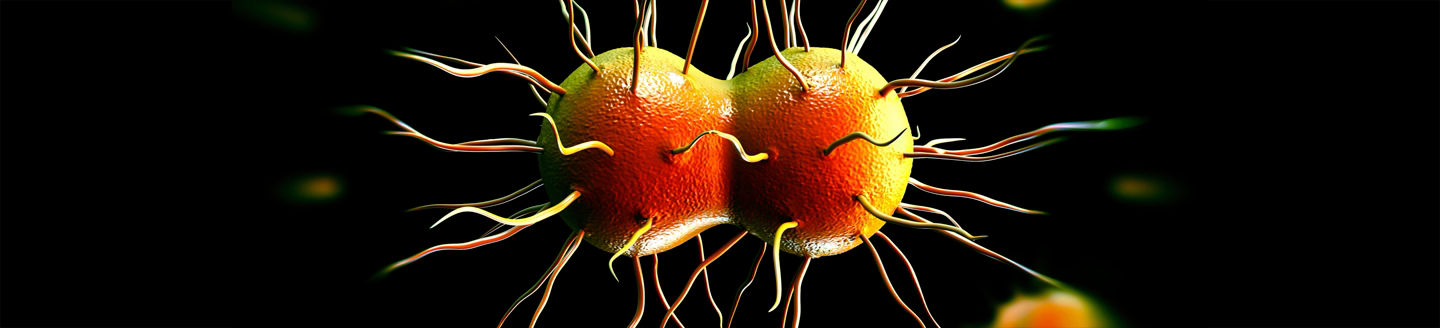
Neisseria gonorrhoeae (NG), also known as gonococcus or GC, is among the most common sexually transmitted infections (STIs), with 87 million new cases annually.1
This bacterial pathogen most commonly causes infection of the throat, anus or urogenital tract, and is acquired through sexual contact. Bacteria invade and attach to host tissue, causing an inflammatory response often leading to a visible discharge.
These bacteria then have the potential to spread upwards through the urogenital tract. This may lead to complications in females that can affect the urethra, cervix, and fallopian tubes. In males, the prostate can be affected. Moreover, these infections may cause infertility for both sexes, along with urogenital symptoms, sores, redness or lesions in the mouth, discomfort, bleeding, or discharge from the anus.
However, the majority of patients do not experience any symptoms at all.