Making up about 80% of an anatomical pathology lab’s work, the hematoxylin and eosin (H&E) stain has become a mainstay as a rapid diagnostic for pathologists.
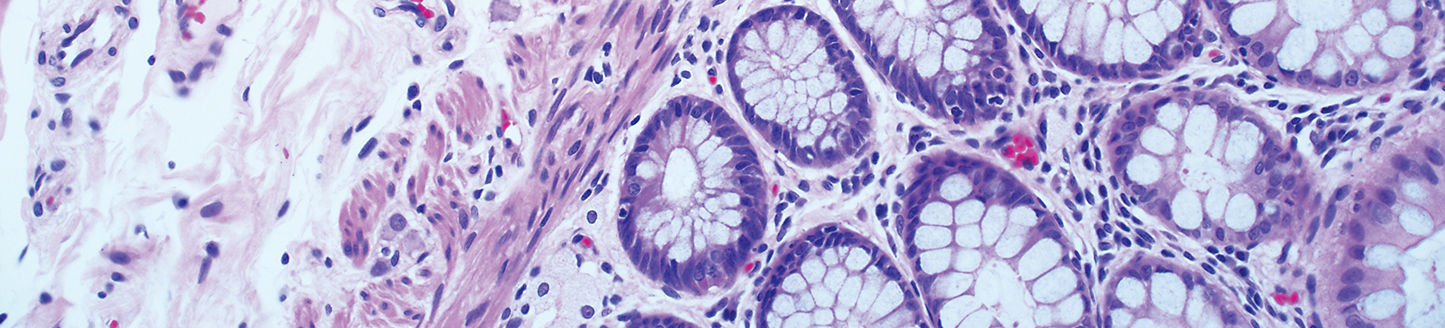
H&E is the principle laboratory method used to examine human tissue specimens for routine diagnosis, setting the course for all further work on patient tissue samples and directing the clinical course for patients. This technique of staining basophilic and acidophilic structures using hematoxylin and eosin, respectively, provides pathologists with functional and morphological details at the cellular level.1
Compared with other histological methods such as immunohistochemistry, H&E is simpler, faster, less expensive and more stable.1,2,3 However, it can be hard to standardize. The appearance and quality of each stain is dependent on numerous factors, such as the type of hematoxylin, the exact staining protocol, the quality of dyes, and their age.4 If the user is able to see what they need for interpretation, the quality is usually considered “satisfactory”, though this may vary by individual.
Despite the well-established utility of the technique, it has remained largely unchanged since its introduction more than a century ago, resulting in high variability between stains.