December 1, 2023
In the fight against diabetes and heart failure, a simple, relatively inexpensive blood test may be key to combating rising incidence rates and improving patient outcomes.
According to the American Diabetes Association (ADA), an estimated 37 million Americans have diabetes, with 28.7 million diagnosed and 8.5 million undiagnosed, and 1.4 million newly diagnosed each year. In 2019, 96 million Americans ages 18 and older had prediabetes.1 And while diabetes presents a host of well-known medical challenges including retinopathy and kidney disease, a diagnosis of heart failure (HF) should be considered early on, even if symptoms aren’t present.
Diabetes increases the risk of developing heart failure
Both Type 1 Diabetes and Type 2 diabetes increase the risk for heart failure, which has been recognized as a common complication in people with diabetes, and may even be their first presentation of cardiovascular disease. Up to 22% of people living with diabetes are estimated to have heart failure. A person with established diabetes (particularly in the presence of other risk factors) should be considered in Stage A HF, and many people with diabetes have Stage B HF.2
“In Stage A, patients are considered ‘at risk’ for heart failure and in Stage B, ‘pre-heart failure,’ as they are beginning to develop heart failure but are asymptomatic,” says Dagmar Schumacher, Ph.D., scientific partner, cardiometabolism, Roche Diagnostics. “In these early stages, certain interventions such as medications and/or lifestyle changes can be made to delay progression to Stage C, which is ‘symptomatic’ heart failure. Heart failure is a progressive, structural disease, so once a patient moves from one stage to the next, there is no going back. Early identification allows for informed decision making around treatment and continued monitoring.”
Early diagnosis with cardiac biomarkers can improve patient outcomes
Predicting risk and detecting heart failure is key to improving patient outcomes, but heart failure in individuals with diabetes is frequently underdiagnosed. Early diagnosis of heart failure could enable targeted treatment to prevent progression of disease and other adverse outcomes.2
According to its consensus report published in Diabetes Care in 2022, the ADA notes “the addition of relatively inexpensive biomarker testing as part of the standard of care may help to refine [heart failure] risk prediction in individuals with diabetes.” The consensus statement, which was endorsed by the American College of Cardiology, also states that “substantial data indicate the ability of these biomarkers to identify those in Stage A or B [heart failure] at highest risk of progressing to symptomatic [heart failure] or death.”2
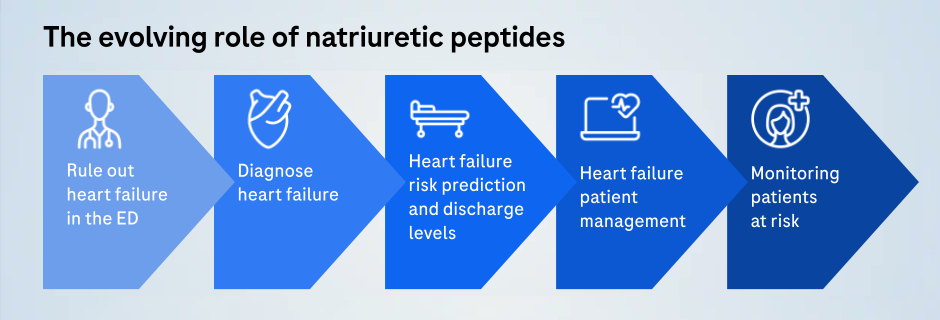
First used as a tool to diagnose acute heart failure in the emergency department (ED), the use of cardiac biomarkers – specifically natriuretic peptides – has evolved over the past two decades. The use of natriuretic peptides to diagnose symptomatic heart failure more broadly soon followed their application in the ED. Their use eventually expanded to include risk prediction – from the acute phase to new acute episodes and ultimately to predicting long-term risk and risk in specific populations, such as people with diabetes.
The ADA recommends individuals with diabetes take a measurement of natriuretic peptides or high-sensitivity troponin on at least a yearly basis to identify the possible presence of Stage B HF and to prognosticate for progression to symptomatic stages of the diagnosis.2
“Cardiac biomarkers, such as NT-proBNP and high-sensitivity troponin, are the most sensitive tools in the toolbox today to detect the onset of wall stress, injury and remodeling of the heart, so we have the opportunity with regular risk assessment to catch if something is off track with our heart at the earliest possible opportunity,” says Schumacher. “Patients with diabetes are at least at a two-fold higher risk of developing heart failure. With the therapies available today, we may be able to prevent progression and at least delay worsening of the condition.”
Reduction in NT-proBNP levels was shown to improve long-term outcomes compared with those who have persistently elevated levels despite appropriate treatment.2 Given the evidence, the potential for improved patient outcomes and the relatively low cost, Schumacher is in support of implementing annual cardiac biomarker testing for people with diabetes.
“If annual cardiac biomarker monitoring is widely adopted when treating people with diabetes, more patients can be appropriately monitored and diagnosed with heart failure earlier in the disease course, leading to improved treatment and delayed disease progression,” says Schumacher. “This should lead to improved quality of life over a longer period of time for these patients.”
Learn more about the American Diabetes Association's recommendations for monitoring heart failure in people with diabetes.