Eradicating cervical cancer will take partnership, policy and medical innovation
October 14, 2024
The statements above are fragments of the thousands of stories from women and people with a cervix impacted by cervical cancer in the U.S. We hear them, we see them and we are moved by them.
We believe that the elimination of cervical cancer is well within reach. As an innovator in cervical-cancer screening, including one of the first FDA-approved HPV self-collection tests,* we at Roche Diagnostics understand that achieving this goal is only possible by partnering with leaders at like-minded organizations who are focused on the needs of women and people with a cervix. We must work with women, healthcare providers and other stakeholders to advance policies that expand access and reduce barriers to screening and diagnostics, as well as continue to develop first-to-market tests that meet the needs of women, their healthcare professionals and their laboratories.
The HPV testing gap
Cervical cancer causes approximately 4,000 deaths in the U.S. each year.1 A key factor behind changing this statistic seems simple – get women screened for cervical cancer. However, about 28% of women are typically not up to date with their screenings.2 And if they are positive for high-risk HPV, many don’t receive the follow-up care they need.


Unfortunately, many reasons exist for not getting screened or getting the appropriate care — ranging from a perceived stigma associated with a sexually transmitted infection to living in a medically underserved area. Cultural sensitivities and modesty or embarrassment related to the exam can also pose barriers to screening.

Additionally, health disparities in cervical-cancer incidence and death related to race, geography, insurance status and gender identity are also a concern. This means some women aren’t getting needed services — notably Hispanic, Black, indigenous and Asian women, those living in rural areas, those who lack insurance and the LGBTQ+ population.3,4
Access is crucial because when invasive cervical cancer is detected at an early stage, the five-year survival rate for women is 91%.5 Not surprisingly, the majority of cervical-cancer cases are found in the underscreened female population. More than half of the women diagnosed with cervical cancer have never been screened or have only been screened infrequently, and they do not participate in routine screening.6
The power of partnerships
Accomplishing a goal as monumental as eliminating cervical cancer takes the work of diverse and dedicated partners across the public and private sectors. No one entity, advocacy group or government can do this alone, and we at Roche are honored to participate in ongoing efforts that mobilize all stakeholders.

We have strengthened our long-standing relationship with Cervivor, the leading cervical-cancer patient advocacy organization. Cervivor is a global community of patient advocates who inspire and empower those affected by cervical cancer by educating and motivating them to use their voices for creating awareness to end stigma, influence decision and change, and end cervical cancer. We partner with Cervivor to extend its innovative and award-winning educational and advocacy training programs to women who have been impacted by cervical cancer and their communities.
Cassandra Ricci, senior manager, Alliance Development and Federal Government Affairs (left) and Tamika Felder at the Cervivor Cervical Cancer Summit in New York, January 2024.
In addition, Roche engaged with women, medical and public health professionals and policymakers at the inaugural White House Cervical Cancer Forum during Cervical Health Awareness Month earlier this year. We discussed ways to improve HPV and cervical-cancer screening rates and how our country has a global role in driving collaboration and progress.
We are also proud to be members of the National Roundtable on Cervical Cancer (NRTCC), created by the American Cancer Society (ACS). Through the NRTCC, we have the opportunity to listen and learn from participating organizations, exchange ideas, and contribute our unique perspective. Earlier this year, we participated in the Self-Collection and Primary HPV Screening Workgroup meetings and discussed the critical health-service delivery considerations for HPV self-collection implementation.
We have a long history of working closely with the World Health Organization (WHO), which has awarded Roche with HPV test and system prequalifications that enable low- and middle-income countries to use Roche HPV screening solutions, including self-collection, in their national cervical cancer elimination programs.
Our partnerships and other collaborations have reaffirmed to us the importance of access to testing, frequently cited as the most important barrier to overcome in eradicating cervical cancer. Our industry has a key role to play in making testing easier and more accessible for all women.
Driving access through medical and public policy
To encourage adoption and implementation of HPV screening and testing innovations, the full health ecosystem – from patient-facing clinicians to advocacy groups to private and public healthcare plans – has to be supportive. In the past few decades, much of this foundation has been set.
Medical societies, advocacy organizations and other expert bodies establish clinical practice guidelines to inform clinical decisions, making it easier for providers to have access to information from evidence-based sources and help them in managing patients. The United States Preventive Services Task Force and the ACS have published screening guidelines that women and providers can use to determine when to start cervical-cancer screening, what types of tests are appropriate and at what intervals. Both of these sets of guidelines highlight the value of HPV testing for cervical cancer.
And in 2024, ASCCP and other members of the Enduring Guidelines for Cervical Cancer Screening and Management recognized dual-stain biomarkers as an important technology in helping clinicians triage women with high-risk HPV. The World Health Organization (WHO) also recognized the value of dual-stain biomarkers in its cervical cancer prevention guideline.
Legislative and policy efforts to address and reduce cancer burden have led to the creation of programs that expand access to screening and diagnostic services in the U.S. In 1991, the Centers for Disease Control and Prevention (CDC) created the National Breast and Cervical Early Detection Program (NBCCEDP). The NBCCEDP helps low-income, uninsured and underinsured women gain access to timely breast- and cervical-cancer screening, diagnostics, and treatment, as well as patient navigation services.
Cervical-cancer screening is among the preventive services covered without patient cost-sharing by the Patient Protection and Affordable Care Act of 2010. Though this policy expanded access to screening for people who could not afford it, experts at the ACS and other organizations believe that the elimination of cost-sharing for people who require additional testing or procedures to determine the presence of cancer or pre-cancer is necessary to fully realize the benefits of cancer screening and early detection.
More than half of the women diagnosed with cervical cancer
have never been screened or have been screened infrequently.6
It is estimated that 20% to 75% of women with an abnormal initial cervical-cancer screening result do not receive essential follow-up diagnostic testing, and eight of 10 women undergoing a colposcopy incurred nontrivial out-of-pocket costs.7 Inadequate cervical-cancer screening rates, coupled with failure to complete recommended follow-up testing and procedures, undermine the opportunity we have to eliminate deaths from this preventable disease.
A recent study, supported by Roche, explored how partial and perfect adherence to screening, surveillance and follow-up diagnostic procedures could potentially affect cervical cancer incidence rates and save lives. By increasing adherence to 100%, the study found that 128 fewer cervical cancers resulted, 62 deaths were prevented and 2,135 life-years were saved per 100,000 women eligible for screening.7 Addressing reasons why women aren’t getting screened, including cultural concerns, social stigma, and financial barriers, could save lives and lead to the U.S. reaching the World Health Organization’s elimination goal of four cases of cervical cancer per 100,000 women.
Medical tools and innovation
Cervical cancer used to be a leading cause of cancer deaths for American women, but thanks to innovation in HPV vaccines and screening tests, rates have dropped by more than half since the mid-1970s.8 Unfortunately, cervical-cancer rates have plateaued over the past decade, which shows that we’re not using the tools we have to prevent, screen, diagnose and treat this cancer to its fullest extent.
With the recent FDA approval that allows women to privately collect their own samples, we believe the diagnostic science is there to fully support women. As a company, we are proud to have led the way with:
- the first FDA-approved HPV primary screening test to detect HPV genotypes at high risk of cancer
- the first and only FDA-approved dual-stain technology test to identify pre-cancer earlier
- one of the first FDA-approved self-collection HPV test,* simultaneously approved with a test from another manufacturer
Roche is participating in the National Cancer Institute’s Self-collection for HPV Testing to Improve Cervical Cancer Prevention (SHIP) trial. We, along with the NIH, believe that this method of self-collection has significant potential to address a persistent cancer disparity by expanding cervical cancer screening access to reach women who are underscreened or never screened. The trial is a network of 25 clinical sites across the US and will serve as an independent platform to evaluate the usability, acceptability and accuracy of multiple self-collection device-assay combinations.

Not every HPV-positive person will develop cervical cancer, so triage is necessary to determine who is most at risk and will benefit from more immediate follow-up, and who is at lower risk and should be given more time to clear the infection naturally. Roche has advanced cervical-cancer screenings by pioneering tests that improve cancer-risk assessment and confirmation, as well as making testing more accessible.
Looking ahead
At Roche, we understand that the tests we develop are meaningful only if they reach the people who need them. We’re hopeful that our recent FDA approval of HPV self-collection,* which makes it possible for women to collect their own vaginal samples in private before handing them off to trained personnel for processing, will help reduce barriers to testing and extend the benefits of screening to women who aren’t currently participating in routine screening.
Initially, self-collection for the Roche HPV test* will take place in a healthcare setting. Over time, increased awareness of self-collection and regulatory approvals could support testing outside of medical settings.
We are clearly at a tipping point in the history of HPV testing and cervical-cancer prevention. The prevention tools exist and stakeholders are aligned. We at Roche remain committed to continuing to work until everyone has access to testing and cervical cancer no longer causes deaths.
*Roche’s HPV self-collection is FDA-approved and is expected to be commercially available in Q4 2024.
Sources
1The National Cancer Institute - Last accessed October 2, 2024
2Center for Disease Control - Last accessed October 2, 2024
3Center for Disease Control - Last accessed October 2, 2024
4National Cancer Institute - Last accessed October 2, 2024
5National Cancer Institute - Last accessed October 2, 2024
6National Cancer Institute - Last accessed October 2, 2024
7Harper, Diane M. MD, MPH; Yu, Tiffany M. BS; Fendrick, A. Mark MD.Lives Saved Through Increasing Adherence to Follow-Up After Abnormal Cervical Cancer Screening Results. O&G Open 1(1):p e001, March 2024.
8American Cancer Society - Last accessed October 2, 2024
Contributors
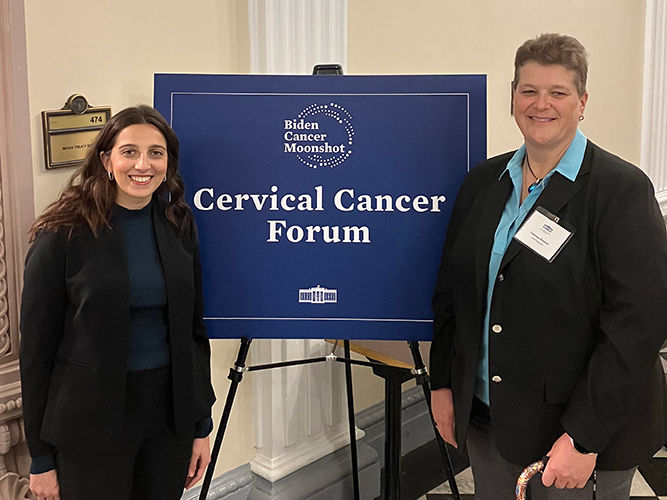
Vanessa Bennett, Roche senior international business leader (right) and Cassandra Ricci, Roche senior manager, alliance development and federal government affairs (left)